Introduction:
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a strain of coronavirus that causes a respiratory illness known as COVID-19. COVID-19 is a pandemic affecting many countries globally.(1) As of 23rd July 2020, there have been 297,146 lab-confirmed cases of COVID-19 in the UK and 45,554 people who tested positive for the virus have died.(2) Patients with multiple myeloma (MM) are at a higher risk of contracting the virus and experiencing more severe outcomes.(3-6) The higher risk is driven by a compromised immune system, the use of immunosuppressive agents and patient characteristics aligning with key risk factors - patients with MM are often elderly and have multiple co-morbidities.(7) In light of the COVID-19 outbreak, NHS England and NICE have issued guidance to modify usual care to reduce patient exposure to COVID-19. For patients with cancer, NICE recommend delivering systemic anti-cancer treatment in different and less immunosuppressive regimens, different locations (ideally at home) or via another (less invasive and/or less resource intensive) route of administration where possible.(8)(9)
The objective of this analysis is to explore the impact of switching patients from intravenous (IV) treatments requiring hospital administrations to subcutaneous (SC) or oral alternatives which can be administered at home or in an outpatient setting which reduces the patient's potential exposure to COVID-19.
Methods:
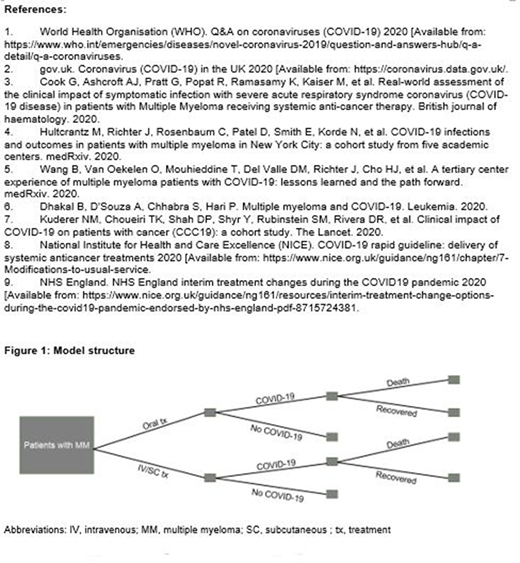
A decision tree model was developed in Microsoft Excel® (Figure 1). Patients enter the model and are assigned a probability of being treated; those that are treated are then assigned a probability of IV, SC or oral-based therapy. Based on the route of administration, patients are assigned a probability of contracting COVID-19 and, for those patients that do contract the virus, a probability of death from the virus is estimated. The model compares the outcomes from two identical decision trees: one informed by the pre-COVID-19 treatment pathway and one informed by the post-COVID-19 pathway. Model inputs, including COVID-19 inputs (e.g., number of active and diseased COVID-19 cases among patients with MM), have been informed by the literature and clinical opinion. Costs reflected in the model include: treatment of COVID-19, treatment for MM and administration of MM treatments. Scenario analyses explore lower and upper bounds for key inputs. Results are presented from a UK perspective and a 1-year time horizon (from model entry) is considered.
Results:
Per the model, treating patients with oral therapies is shown to reduce the number of COVID-19 cases and the number of COVID-19 deaths in patients with MM compared with IV- and SC-delivered therapies. These outcomes translate into cost savings driven by costs avoided in treating COVID-19. There was a limited difference in the costs of treating the underlying MM despite the switch. However, there were additional cost savings demonstrated through avoiding expensive and resource intensive administration appointments associated with IV therapies, and to a lesser extent SC therapies. The use of oral therapies has also aided the increase in telemedicine for routine appointments - scenarios exploring this demonstrate further savings. These results are driven by the perceived risk attached to each of the different routes of administration - scenario analyses demonstrated that assuming even the lower bound risk (an assumed additional risk of 10%) for IV therapies vs. oral therapies, a significant number of COVID-19 cases and deaths were avoided, and costs reduced.
Conclusions:
Changes to the treatment pathway for patients with MM in light of the COVID-19 pandemic aim to reduce the exposure to the virus for these patients. The model demonstrates that simply switching the route of administration can reduce the number of COVID-19 cases and deaths . This has important implications in avoiding severe outcomes, decreasing the spread of the virus and reducing the cost and resource use burden to the healthcare system. In addition, the model reflects potential efficiencies which may extend beyond the COVID-19 pandemic (e.g. telemedicine) to optimize clinical practice for patients with MM in the longer-term.
Cranmer:Takeda: Current Employment. Podkonjak:Takeda: Current Employment. Benson:Takeda: Current Employment. Dabora:Takeda: Current Employment. Jackson:Merck Sharp and Dohme: Honoraria; Chugai: Honoraria; Amgen: Honoraria; Janssen: Honoraria; Celgene: Honoraria; Takeda: Honoraria; Roche: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal